Gene editing to change SMN2 gene into SMN1 shows promise in mice
A single gene-editing treatment that converts the SMN2 gene into a functioning copy of SMN1 increased levels of the SMN protein that is lacking in spinal muscular atrophy (SMA), bringing better motor function to a mouse model of the disease, a study reported.
Combined with Spinraza (nusinersen), an approved SMA injection therapy, the gene-editing treatment fully restored the animals’ muscle strength, coordination, and physical activity, and extended their lifespan.
“One of the real promises of precision gene-editing therapies is the possibility that a one-time treatment can provide a therapy for the lifetime of the patient,” David Liu, PhD, a professor at the Broad Institute of Massachusetts Institute of Technology and Harvard University and the study’s lead author, said in a university press release.
The approach was detailed in the study “Base editing rescue of spinal muscular atrophy in cells and in mice,” published in the journal Science.
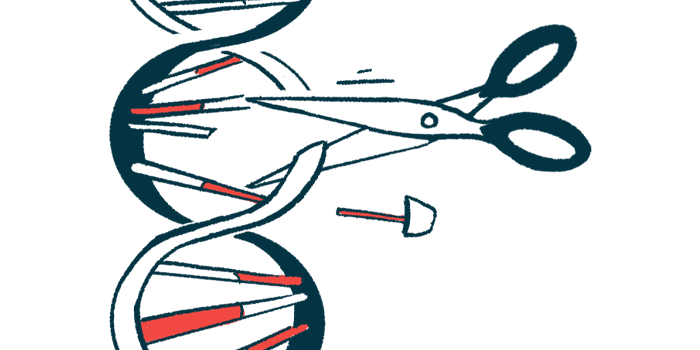
Gene editing to correct single letter change in SMN2 gene’s DNA sequence
Mutations in the SMN1 gene are the common cause of SMA, leading to little or no SMN protein production and the progressive loss of motor neurons, the nerve cells that control movement.
Cells also can carry the “backup” SMN2 gene that encodes for this protein, and a patient’s number of SMN2 gene copies is generally associated with greater SMN production and a milder SMA type.
Due to a single base — or letter — change in the DNA sequence of SMN2, however, cells produce a shorter version of the SMN protein that degrades quickly and fails to fully compensate for the loss of SMN1.
Working with scientists at other institutes in Massachusetts and Ohio, Liu set out to design a gene-editing tool capable of replacing the single letter change in SMN2’s DNA sequence. The team’s goal was to convert SMN2 into a working copy of SMN1 with greater SMN protein production.
“Base editing is a powerful tool to correct genetic diseases,” said Mandana Arbab, PhD, a postdoctoral fellow in Liu’s lab and the study’s co-first author. “Most drugs find ways to compensate for what has already gone wrong in a cell, but here we use base editing to stop SMA where it originates, in the DNA.”
The scientists evaluated 79 different gene-editing strategies using machine learning and lab tests. One was seen to restore SMN production with few off-target DNA edits, which carry a potential for side effects. This strategy raised SMN protein levels 40 times, they reported, reaching levels similar to those found in healthy cells.
In an SMA mouse model, the gene-editing tool was delivered to the brain and spinal cord using a modified, harmless virus. Tests showed about 43% of motor neurons in the spinal cord received the molecules required for gene editing, and 87% of those had SMN2 to SMN1 conversion.
Gene-editing treatment plus Spinraza restored muscle strength, activity
Similar, or even greater, motor gains were seen in comparing the gene editing treatment with the three approved SMA treatments: Spinraza, an intrathecal (spinal cord) injection treatment; Evrysdi (risdiplam), an oral daily therapy; and Zolgensma, a one-time gene therapy.
Spinraza and Evrysdi are designed to correct SMN2 at the RNA level to increase the production of a full SMN protein. RNA is the intermediate molecule that’s produced from DNA and serves as a template for protein production. Zolgensma uses an engineered virus to carry a working copy of SMN1 to cells.
“The three FDA-approved drugs have revolutionized the treatment of SMA for thousands of patients,” Liu said.
Notably, SMA model mice treated with a single dose of the gene-editing treatment plus Spinraza showed no significant differences to healthy mice in muscle strength, coordination, and physical activity. Treated SMA mice also lived 6.5 times longer on average than untreated animals (111 vs. 17 days).
“These findings demonstrate the potential of a one-time base editing treatment for SMA,” the team wrote.
Researchers suggested that Spinraza may have extended the time when motor neurons can be rescued, allowing the gene-editing treatment more time for SMN2 to SMN1 conversion. Because this period is longer in people than in mice, occurring over months rather than days, Liu suggested the editing treatment may be more effective in patients, especially in combination with current SMA therapies.
Liu’s lab is working on a different viral delivery system, one that could potentially reduce the dose and simplify their gene editing approach for SMA.
“There’s still a huge amount of work to do,” Liu said. “But achieving a good understanding of how many different gene editing strategies each affect SMA is an important start to our no-stone-unturned approach to developing one-time treatments for SMA and other serious genetic diseases.”
Funding for the study was provided in part by the National Institutes of Health, the Howard Hughes Medical Institute, the Bill and Melinda Gates Foundation, and the Friedreich’s Ataxia Research Alliance (FARA).
The post Gene editing to change SMN2 gene into SMN1 shows promise in mice appeared first on SMA News Today.