SMA Patients May Have Difficulties Laying on Their Stomachs
When patients are limited in their range of motion, this can lead to an inability to tolerate certain positions. For example, Michael, who has been diagnosed from an early age with SMA, is severely lacking hip and knee extension, making it hard for him to assume a prone position. This is due to a few different contributing factors; first and foremost being that he sits in a wheelchair for the majority of his day, which he has done for many years. This has caused his muscle to form contractures or tightening of the muscles and led them to shorten and become stiff. Another factor that limits his range of motion, in general, is having a spinal fusion. With all of these limitations, it has been nearly impossible for Michael to attempt to position himself in a prone, or face down, position. This is a position that used to be very comfortable for Michael to sleep in, but he hasn’t been able to do this since his back surgery in 1980.
With improvements being made in his hip and knee extension, as well as with new equipment available to us at my new outpatient clinic location, one being an oversized high low therapy table, this topic has become something that we could begin to work on. Most of the time we discuss things two weeks in advance that we may try during the next visit, but placing Michael in a prone position has been something he has wanted to be able to try for a long time. Recently, at one of his appointments, he mentioned this again in conversation. We were already in a supine position transferred onto the therapy table, so we decided to go ahead and give it a try.
The most challenging part was figuring out how to position his head secondary to the lack of range of motion of his cervical and thoracic spine. Because of the lack of cervical mobility, I knew Michael wouldn’t be able to sustain a position in which his neck was rotated to the side with his cheek on the table. I would usually use a face pillow in this instance, but I also knew that Michael wouldn’t be able to perform any thoracic extension to position himself onto a face pillow. For the first attempt, we used a towel roll under his right shoulder after we got him rolled over to try and keep his shoulder from moving under him. His cervical spine was as rotated as he could maintain looking to the left and we placed pillows under his hips to try and make it as comfortable as we could, while still getting a stretch in his anterior hip musculature.
While in this position, I checked on Michael frequently to get his feedback and make sure he wasn’t uncomfortable. I then placed one hand on his posterior hip and the other under his anterior knee and pulled into extension to increase the stretch. After this session, there was more brainstorming performed with the massage therapist who assists me. We put together a few square steps that have holes in the middle of them and used a U-shaped pregnancy pillow on the top to form a flat face pillow right off of the table. Therefore, we could roll Michael onto his stomach with his head maintaining a forward-facing position with no extension needed. In this position, he would be more likely to tolerate a prone position for a prolonged period, and we could take advantage of the new position to attempt new activities.
After positioning Michael in a prone position and doing his hip extensions, we concluded that even though Michael could tolerate being placed in a prone position, it would be more comfortable for Michael to continue performing this exercise in a supine or side-lying position for now. In these positions, we can control his range of motion with more stability and control. As we continue to attempt new positions and activities, this prone position will be revisited at another time.

I feel it’s very important for any physical therapist to understand that just because you feel that the equipment you have won’t work for positioning a particular patient, doesn’t mean you should just give up and tell the patient no. Work together with them, get their feedback. Let them be a part of their treatment and brainstorm with them. Discuss how the transition will work and what difficulties you think they may have, and how you can help them to overcome some of these challenges. If it is important to your patient, it should be important to you.
======================== Patient Perspective ========================

For those of you that know me, you know that I’m probably one of the most optimistic and positive people that you will meet. I never look at the glass as being half-empty.
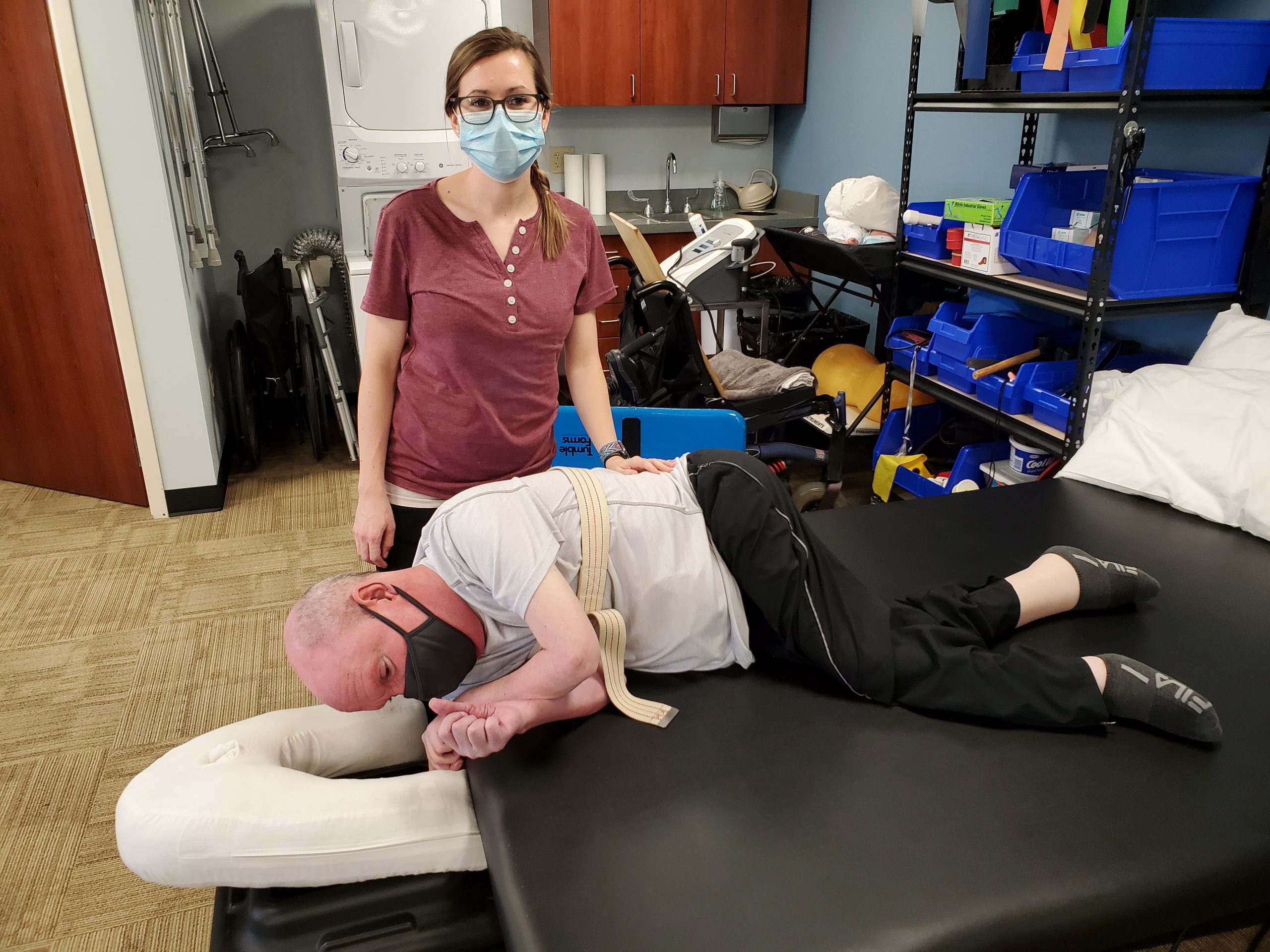
During physical therapy a couple weeks ago, my physical therapist, Emily, worked with me on getting me in a prone position. The last time that I was on my stomach was when I was 14 years old. Emily and my other PTs have been working very hard on improving my flexibility and range of motion in my hips, and I thought I would be able to get on my stomach without too much difficulty. While they were able to get me on my stomach, the picture that they took completely devastated me. After looking at this picture, it quickly reminded me how much this disease has ravaged my body. It actually took me a few days to come to terms with even sharing this picture in this article.
While I know I shouldn’t be embarrassed about this picture, I am. When I was on my stomach, it felt as if my legs were stretched out and flat on the table, but as you can see by the picture, they were anything but stretched out. While this picture is difficult for me to look at, it reminds me that I still have a lot of work to do. I may not ever get to the point where I can stretch out flat, and that’s okay, but my prayers and hopes are that we can improve my flexibility and range of motion over the coming years so that I can replace this picture with one that doesn’t look as bad as this one.
Setting goals, even long-term goals, is something we all should do, and I’m going to do everything in my power to reach this goal.
Emily and all of my PTs have never given up on me, and I refuse to give up on myself.



