Safety For Both Therapist and SMA Patient

While working with a patient with SMA, you may find it beneficial for the patient, as well as the therapist, to have at least two people available to help in the treatment if you plan to transfer to a therapy table for different exercises. For Michael, we transfer him from his wheelchair to the therapy table every other week to perform seated balance activities as well as stretching of his lower extremities.
During these activities, having at least two people to work with Michael, allows for increased safety for the patient and therapist, as it allows the therapist to have better body mechanics and the patient to have optimal guarding. Although these transfers and exercises are possible to complete with one person when necessary, this is not always ideal. When we transfer Michael from his chair to the table, we use a slide board. We utilize a max transfer x2 to ensure Michael’s safety, as well as to ensure that all of the therapists maintain good body mechanics to decrease the risk of injury. It is best to have one therapist control Michael’s upper body and to safely lean him to his side to allow for slide board placement, while the other therapist places the slide board and controls his hips to allow for quick removal of slide board, secondary to nerve damage in Michael’s hip.


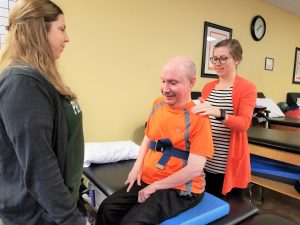
While seated on the therapy table, it is unsafe to have only one therapist perform seated balance activities. For safety reasons, we have one therapist stand in front of Michael, and one therapist stands behind him. This not only ensures Michael’s safety if he loses his balance during these perturbation exercises, but it also gives Michael peace of mind. When transferring Michael from a sitting to a supine position, it is optimal to have one therapist control his upper body, while the other therapist controls his lower body during the transfer to increase safety. It is possible to perform this with one therapist, although it may be uncomfortable for Michael, secondary to a past knee injury and lack of control of his lower extremities to perform upper and lower body separately during the transfer.

Performing hip and knee extension as well as dorsiflexion is easily accomplished safely with one therapist, although having two therapists allows for working on both legs at the same time to increase efficiency with the time we have. There is one safety concern with this exercise when performing hip extension on Michael’s right lower extremity. Due to decreased flexibility, Michael tends to begin to lean to the left with increased stretch. While it is okay to stop the stretch and correct his posture with one therapist, it allows for increased stretch for prolonged periods if there is another therapist there to assist. Stretching of the hip flexors can be performed in many ways, although we have discovered that Michael receives a better stretch of his hip flexors in a side-lying position. While rolling from side to side, it is optimal to have one person on each side of the therapy table to allow for safety and ensure there is enough room on each side to safely roll onto his side. This would be done efficiently with one person if you have an oversized therapy table but is difficult with one therapist on a standard-sized table.


This stretch is possible to perform with one therapist, although having two therapists allows for improved body mechanics for the therapist as well as improved ability to guard Michael’s upper body while performing this activity. As pictured, due to his decreased hip flexor length, it’s best to have one therapist guard in front and maintain hip position, while another therapist uses body weight to pull back on his lower extremity and manipulate knee flexion to decrease or increase quadricep involvement.


Although it is possible to treat a patient with SMA with one therapist effectively, to ensure the safety of the patient and therapist, if possible, allow for more than one therapist to be available during these activities. Although this is not cost-effective, it truly can be what is best for the patient, and that should be our number one goal. I would encourage each therapist to take their time and think through each move and communicate to the patient along the way so they know what to expect, and trust that you are confident in what you are doing and are ensuring their safety and wellbeing along the way.

