Ultrasound-aided Spinraza injection cuts needle redirections: Study
The use of ultrasound to guide the administration of Spinraza (nusinersen) injection into the spinal canals of adults with spinal muscle atrophy (SMA) significantly reduced the number of needle redirections compared with a standard, landmark-based approach, according to a clinical trial.
Among patients with spinal deformities, ultrasound helped reduce needle redirections — a process that involves carefully withdrawing the needle slightly while maintaining its position in the skin, then redirecting its angle and reinserting it — even further.
Nevertheless, the number of successful treatment attempts, procedural time, patient satisfaction, and the incidence of adverse events were similar for both procedures.
“These results suggest that the [ultrasound] assistance may be advantageous for Spinraza therapy to reduce the therapeutic burden of [spinal canal] infusion,” the researchers wrote.
The study, “Ultrasound assisted versus landmark based intrathecal administration of nusinersen in adults with spinal muscular atrophy disease: A randomized trial,” was published in Muscle & Nerve.
Spinraza injection may be a challenge
Spinraza is an approved therapy for all types of SMA. It works by boosting the production of SMN, a protein essential for the health of motor neurons that is lacking in SMA patients due to mutations in the SMN1 gene. After an initial loading period of four doses, patients routinely receive Spinraza once every four months.
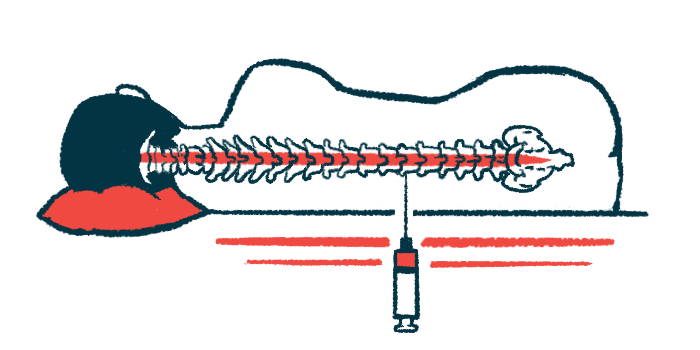
The therapy is administered directly into the spinal canal, a procedure called an intrathecal injection. Typically, specific anatomical landmarks on a patient’s back help guide the needle’s insertion into the spinal canal.
This route of administration can be challenging in very young SMA patients and/or those with scoliosis, a sideways curvature of the spine, and/or previous back surgery.
Ultrasound, also called sonography, has been used to guide intrathecal injections in SMA patients with complex spines. The noninvasive technique uses high-frequency sound waves to view soft tissues such as muscles and internal organs.
A team of researchers in Italy conducted a clinical trial (NCT04674618) to determine whether ultrasound could reduce the number of needle attempts needed for successful drug administration compared with the conventional landmark-based technique.
A total of 58 adult SMA patients were randomly assigned to receive Spinraza injections via a landmark-based or ultrasound-assisted technique. Slightly fewer than half of the patients in both groups (44.8%) had a spine deformity due to corrected or uncorrected scoliosis.
Secondary outcomes included the number of needle redirections needed for intrathecal drug administration, procedural time, patient satisfaction, and the incidence of adverse events.
Ultrasound approach seen effective, safe
Spinraza was successfully administered in 28 of 29 patients in the ultrasound group and 27 of 29 patients in the landmark group. The number of attempts needed to reach the spinal canal was low and similar between the ultrasound and landmark groups.
Still, the number of needle redirections was significantly lower using ultrasound versus the landmark-based technique. The mean procedural time was about 40 seconds longer in the ultrasound group. Patient satisfaction between the two groups was similar, and there was no difference in the occurrence of adverse events such as low back pain and headache.
Among the 26 patients with a challenging spine deformity, the number of successful administration attempts was similar between the ultrasound and landmark groups (92.3% vs. 84.6%). No difference in procedural time was noted in this subgroup. However, the mean number of needle redirections was more pronounced in the landmark group than in the ultrasound group (6 vs. 2).
The team then examined the relationship between the number of needle redirections and Cobb’s angle, the degree of sideways spinal curvature, with higher values indicating more severe scoliosis. As expected, a greater Cobb’s angle resulted in more needle redirections, but the increase was significantly higher for landmark procedures than for ultrasound procedures.
“In adult patients with SMA, both the anatomical landmark-based technique and the [ultrasound]-assisted technique are effective and safe,” the researchers concluded. “The use of [ultrasound]-assistance reduces the number of needle redirections needed for intrathecal drug administration in all patients, and in particular in those with complex spines.”
The post Ultrasound-aided Spinraza injection cuts needle redirections: Study appeared first on SMA News Today.





